Showing posts with label Metabolic System. Show all posts
Showing posts with label Metabolic System. Show all posts
Friday, June 16, 2017
Hyperventilation - Causes And Management
Hyperventilation is breathing which occurs more deeply and/or more rapidly than normal.
Pathophysiology: CO 2 is ‘blown off ’, so that pCO 2 decreases.. Hyperventilation may be primary (‘psychogenic’) or secondary. A classical secondary cause is DKA — Kussmaul’s respiration represents respiratory compensation for a metabolic acidosis.
Secondary causes of hyperventilation
• Metabolic acidosis (eg DKA, uraemia, sepsis, hepatic failure).
• Poisoning (eg aspirin, methanol, CO, cyanide, ethylene glycol).
• Pain/hypoxia.
• Hypovolaemia.
• Respiratory disorders (eg PE, asthma, pneumothorax).
Primary (psychogenic or inappropriate) hyperventilation
Typically, the patient is agitated and distressed with a past history of panic attacks or episodes of hyperventilation. They may complain of dizziness, circumoral paraesthesia, carpopedal spasm, and occasionally sharp or stabbing chest pain. Initial examination reveals tachypnoea with equal
air entry over both lung fields, and no wheeze or evidence of airway obstruction.
Thursday, May 18, 2017
Introduction to Metabolic Acidosis
Metabolic acidosis is more prevalent among children, who are vulnerable to acid-base imbalance because their metabolic rates are faster and their ratios of water to total body weight are lower. Severe or untreated metabolic acidosis can be fatal.
Etiology
Metabolic acidosis usually results from excessive burning of fats in the absence of usable carbohydrates. This can be caused by diabetic ketoacidosis, chronic alcoholism, malnutrition, or a low-carbohydrate, high-fat diet—all of which produce more keto acids than the metabolic process can handle.
Other causes include:
- anaerobic carbohydrate metabolism: a decrease in tissue oxygenation or perfusion, as occurs with pump failure after myocardial infarction, or when pulmonary or hepatic disease, shock, or anemia forces a shift from aerobic to anaerobic metabolism, causing a corresponding rise in the lactic acid level
- renal insufficiency and failure (renal acidosis): underexcretion of metabolized acids or the inability to conserve base
- diarrhea and intestinal malabsorption: loss of sodium bicarbonate from the intestines, causing the bicarbonate buffer system to shift to the acidic side. For example, ureteroenterostomy and Crohn’s disease can also induce metabolic acidosis.
Introduction to Metabolic Alkalosis
Etiology
Metabolic alkalosis results from loss of acid, retention of base, or renal mechanisms associated with decreased serum levels of potassium and chloride.
Loss of acid
Causes of critical acid loss include vomiting, nasogastric tube drainage or lavage without adequate electrolyte replacement, fistulas, and the use of steroids and certain diuretics (furosemide, thiazides, and ethacrynic acid).
Hyperadrenocorticism is another cause of severe acid loss. Cushing’s disease, primary hyperaldosteronism, and Bartter’s syndrome, for example, all lead to retention of sodium and chloride and urinary loss of potassium and hydrogen.
Retention of base
Excessive retention of base can result from excessive intake of bicarbonate of soda or other antacids (usually for treatment of gastritis or peptic ulcer), excessive intake of absorbable alkali (as in milk-alkali syndrome), administration of excessive amounts of I.V. fluids with high concentrations of bicarbonate or lactate, or respiratory insufficiency—all of which cause chronic hypercapnia from high levels of plasma bicarbonate.
Tuesday, May 16, 2017
Introduction to Glycogen storage disease
Normally, muscle and liver cells store glycogen. Muscle glycogen is used in muscle contraction; liver glycogen can be converted into free glucose, which can then diffuse out of the liver cells to increase blood glucose levels.
Glycogen storage disease manifests as a dysfunction of the liver, heart, or musculoskeletal system. Symptoms vary from mild and easily controlled hypoglycemia to severe organ involvement that may lead to cardiac and respiratory failure.
Causes
Almost all glycogen storage disease (types I through V and type VII) is transmitted as autosomal recessive traits. The mode of transmission of type VI is unknown; type VIII may be an X-linked trait.
The most common type of glycogen storage disease is type I, glucose-6-phosphatase deficiency, or von Gierke’s disease, which results from a deficiency of the liver enzyme glucose-6-phosphatase. It occurs in about 1 in 200,000 births, but the incidence may be higher in some populations. This enzyme converts glucose-6-phosphate into free glucose and is necessary for the release of stored glycogen and glucose into the bloodstream to relieve hypoglycemia.
Infants may die of acidosis before age 2; if they survive past this age, with proper treatment, they may grow normally and live to adulthood with only minimal hepatomegaly. Brief periods of fasting may produce irritability due to hypoglycemia and acidosis. Perspiration is excessive, and older children show heat intolerance. Easy bruising may be common. In older, untreated children, growth may be slow and sexual development may be incomplete. Hepatic adenomas are commonly seen by adolescence and may be premalignant lesions.
Signs and symptoms
Primary clinical features of liver glycogen storage disease (types I, III, IV, VI, and VIII) are hepatomegaly and rapid onset of hypoglycemia and acidosis when food is withheld. Symptoms of muscle glycogen storage disease (types II, V, and VII) include poor muscle tone; type II may result in death from heart failure.
In addition, type I may produce the following symptoms:
Tuesday, April 25, 2017
Thiamine (Vitamin B1) Deficiency and Wernicke-Korsakoff Syndrome
Thiamine is absorbed readily in the upper small bowel. Increased requirements are seen in pregnancy, lactation, thyrotoxicosis, and fever. Increased losses are seen with diuretic therapy and peritoneal dialysis.
Clinical Features: Thiamine deficiency causes syndromes affecting the cardiovascular and neurologic systems. They are better known by the names beriberi and Wernicke-Korsakoff syndrome. There are two forms of beriberi, wet and dry.
In developed countries, thiamine deficiency is seen mostly in chronic alcoholics. However, it has been reported to occur in others, such as pregnant women with hyperemesis gravidarum on prolonged intravenous fluid therapy, patients on parenteral nutrition, and elderly patients. In alcoholics, thiamine deficiency is due to decreased intake consequent upon a poor diet and also decreased absorption from the intestine.
Neurologic and cardiovascular manifestations are the common presenting symptoms of thiamine deficiency.
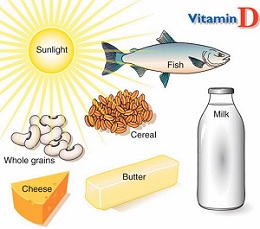
Introduction To Vitamin D Deficiency
Sources Of Vitamin D:There are two forms of Vitamin D known as D2 and D3.
- Vitamin D2 also known as Ergocalciferol basically comes from fortified foods, plant foods and supplements.
- VitaminD3 also known as Cholecalciferol comes from fortified foods, Animal sources like fish, eggs and liver as well as can be synthesized in the body when the skin is exposed to ultraviolet rays from the sun.
Mild deficiency of Vitamin D is usually not associated with any symptoms. The main symptoms are bone pain and muscle weakness. The deficiency of Vitamin D is associated with a number of different health disorders like:
- Rickets in children characterized by impaired growth and deformity of long bones.
- Osteomalacia in adults characterized by muscle weakness and bone fragility
- Osteoporosis a condition with reduced bone mineral density and increased risk of fractures.
- Increased risk of death from cardiovascular disease.
- Cognitive impairment in older adults
- Muscle twitching or fasciculations .
- Severe asthma in children
- Increased risk of cancer.
- Increased chanced of being diagnosed with Schizophrenia
Managing Vitamin D Deficiency
Diagnosis Of Vitamin D Deficiency:
A low level of Vitamin D can be diagnosed with a blood test that checks the levels of 25 hydroxyvitamin D:
- A normal level is defined as a concentration greater than 30 ng/ml
- Insufficiency is defined as levels b/w 20-30 ng/ml
- Deficiency is defined as levels less than 20 ng/ml
The amount of vitamin D that is needed to correct the deficiency depends upon the severity of the deficiency.
Rule of thumb: for every 1 ng/ml increase in your blood level you need an additional 100 IU vitamin D per day.
Subscribe to:
Posts (Atom)